How did you find out about your child’s diagnosis? Tell us about your experience pre-diagnosis including symptoms and doctor’s visits.
In the spring of 2019, Evan started to have some issues with balance and was tripping and falling a lot. He also started having some emotional difficulties such as frequent crying and meltdowns, which was very unusual for him. In the few weeks prior to his diagnosis, he also developed some drooling, slurred speech, lethargy, and headaches. We brought Evan to our local pediatrician and thankfully, he took things very seriously and advised us to go to the emergency room in order to expedite an MRI. That same day, we went to Barbara Bush Children’s hospital in Portland, ME and our nightmare began. Evan did have an MRI at 9pm that night, which they told us would be about 45 minutes. After two hours had passed, we just knew something was really wrong. After the MRI, close to midnight, we were called into a conference room with a pediatric doctor that was there that night. She told us that she had “bad news” for us and that Evan had a brain tumor. She showed us the slides from the MRI and pointed out the tumor, but said since was not a neurologist, she couldn’t really provide us with any further information, and we would have to wait until the morning to meet with a specialist.
What did receiving the devastating news of your child’s serious illness feel like for your family?
After finding out that Evan had a brain tumor, we were in complete shock. We obviously knew that something was going on with him, but honestly never considered this. The following morning, we were again pulled into a conference room with an oncologist, palliative care doctor, and a social worker. It was then that we found out that not only did Evan have a cancerous brain tumor, due to its location in the brain stem, it was considered inoperable, that chemotherapy was not an option, and that palliative care (radiation) was the only option. We were told he had approximately 9 months to live. I think this was the worst day of our lives; learning that our son had cancer and that there was nothing we could do to save him was just absolutely devastating. It’s something no parent should ever have to live through. Two days later, Evan had a brain biopsy surgery and spent the rest of the week in the hospital.
How did your child’s treatment progress? Describe one or two of the hardest moments. If you can, tell us a bit about their final days and end of life.
In August of 2019, Evan began his first round of radiation, which would be for 30 days. Because he was only five, our team insisted that he needed to be sedated for each treatment, which also meant having a port surgically implanted prior to starting radiation. Each morning we had to be at the hospital, which was an hour away, for 7 am. About two weeks into radiation, Evan’s port became infected and he had to have it removed and was hospitalized for another week and received IV antibiotics, for which he needed a PICC line. Fortunately the infection was able to be treated and he was discharged with home IV antibiotics, which he would need for several weeks. I don’t recall a home health nurse ever coming during this time, other than an initial visit, which meant that Brent and I were responsible for running the pump and flushing out his PICC line daily. Evan did remarkably well with radiation. He started to improve drastically about halfway through and had almost complete symptom resolution. Evan was able to begin kindergarten at the end of September 2019, something that we never thought he would do. Evan also started a targeted oral chemotherapy medication at that time.
Over the next three years, we really tried to live every day to the fullest, which was difficult because we were experiencing anticipatory grief, along with considerable anxiety around when Evan’s symptoms would begin to come back. Despite the pandemic, we traveled all over the country as a family and went on as many adventures as we could. When Evan was first diagnosed, I stopped working and Brent began working from home full-time, this meant that we got to spend a lot of time together as a family, which we really enjoyed and cherished.
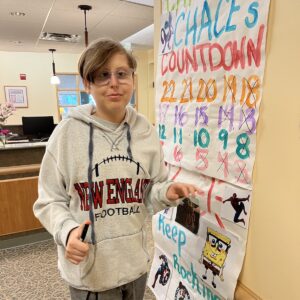
After about a year, Evan began having some symptoms again. After much debate, we opted for a second round of radiation, which was 20 courses. Our medical team was hopeful that Evan would respond well, since he had the first time, but it was not without considerable risk. Evan completed a second course of radiation right after Christmas of 2020. This time, we advocated for Evan to be awake during radiation as we did not want to take the chance on another port or PICC line. Evan was the first child to have radiation awake at Maine Medical Center, and he did so well! He was so brave, it was really amazing, but I guess not really surprising given the special kid that he was. He again responded very well and was able to return to school and even got to play on the town baseball team that summer. Shortly after completing radiation, Evan was started on a new trial medication for which we had to travel to Rochester, NY every other month to obtain.
In December of 2021, Evan started to decline quickly. We had just started him on a new oral chemo combination a few months before, but it was not helping. In just a few weeks, he went from going to school, playing and eating, to becoming so unstable that he was unable to walk without assistance, could no longer eat solid foods and was having difficulty speaking. This was a very scary time as we knew that we were likely out of options at this point. We ended up starting Evan on steroids again, which we always said we would never do because of the horrendous side effects, but they did help his neurological symptoms for a short time. Evan also underwent a third, short course of radiation as an attempt to stabilize the tumor. He also started Avastin, which is an IV chemotherapy type drug that can help reduce swelling in the brain. We continued this for a few months, until it became too difficult for Evan to travel to Portland. Over the next few months, Evan lost his ability to eat, speak, walk, use his left arm, and no long had fine motor skills. He also gained about 20 pounds in just a few short months because of the steroids, which caused him to have really bad stretch marks on his stomach, that eventually split open. These were very painful and required wound care and daily dressing changes.
Because of all the side effects, in April of 2021 we decided to discontinue steroids. This was a very difficult decision as we knew that he would likely decline from a neurological standpoint quickly. Instead, for a short time, the opposite happened. Evan’s mood improved dramatically and he began laughing and trying to smile again, and his speech also noticeably improved. We really maximized this time that he was feeling better and went on a few long weekends, saw friends, took him to our daughter’s sporting events, and even took a trip to Florida! I remember we went to Vermont to be with Brent’s family for Memorial Day Weekend and he was still in good spirits, but the following week started to decline quickly. Evan could no longer swallow or take in anything by mouth, so we opted for a feeding tube procedure. Shortly after that, his heart rate began to sky rocket and then his oxygen levels began to drop and he needed to be on continuous oxygen. The night of June 8th, Evan had gone to bed and woke up shortly after complaining of extreme thirst, but since he was unable to swallow without choking, this was very difficult to manage. All night we were giving him drops of gatorade with a syringe, but he would eventually start choking, so we would have to use the suction machine and then also use a nebulizer to clear out his lungs. At this point Evan was regularly using morphine, so the next morning our hospice nurse suggested to give him another dose of morphine and some Ativan to calm him down. He fell asleep on the couch in the living room and would never wake up again.
We spent the day snuggling with him on the couch and friends and family stopped by to see him and say goodbye. That night, my husband had the foresight that Evan would likely pass away, so we all decided to camp out in the living room with him. Evan’s heart rate continued to sky rocket and around 1am his breathing pattern changed and he took his last breaths. The three of us were holding him and it was an extremely peaceful transition. As strange as this sounds, it was how we hoped it would be for him. In some ways I felt very similar emotions as I did when he was born, which was just essentially an immense amount of love, only paired with sorrow instead of joy. We changed him into his favorite Super Evan shirt and wrapped him up in a special blanket given to him by friends. The next morning, family returned to be with him and we were able to keep him home with us until the funeral home came around 9 am.
What made your child unique? What were some of your child’s favorite things to do during treatment? Did they have heroes, sources of comfort & joy?
Evan really defied all of the odds from the beginning. When Evan was first diagnosed, we were told he would only live for about 9 months, but he not only lived, but really thrived for almost three years. I think this may partly be due to all of the alternative therapies that we tried, including a strict Keto diet, high dose cannabis, hyperbaric oxygen therapy and multiple supplements. I think the other part was Evan’s spirit. He was such a happy kid all the time. He knew that he had cancer, but he had no idea that he was going to die. One thing that brought Evan a lot of comfort the last few months was seeing his friends. We had people sign up to come over and read to him and we had LOTS of visitors, it was really wonderful. The other main source of comfort was always doing Lego sets. We spent so much time putting Lego sets together, and when he was no longer able to help, he would sit and watch us put them together. Evan was filled with so much joy and he LOVED life, his friends, and his family so much.
How are you dealing with your grief? How are your surviving children or partner managing now? What are some of the things that help your family keep going?
After Evan passed, I think we all felt a small sense of relief that he wasn’t suffering anymore and were somewhat in shock/numb. Now that some time has passed, it just seems like it’s getting harder. The realization that we are never going to see him again has really set in. We just miss him so much and think about him nearly every second of every day. We keep going because there really is no other option. It certainly isn’t easy, but we know that our daughter needs us and we want her to have the life she deserves. We also want to live a life that would make Evan proud.
Do you have any advice for a family facing the end-of-life of their child? What helped you most? Are there any organizations that we can share as resources to other families?
I think the biggest thing for us was focusing on quality of life at all times. We always did what we thought was best for Evan and tried not to let our own emotions get in the way of this. I also think it’s really important that you can hold on to hope and still accept that your child is going to die, and accepting this does not mean you are “giving up.” We also knew that we were living on borrowed time, and that was how we lived.
One of our favorite organizations (aside from Rett’s Roost) is The MaxLove Project. Their mission is helping kids and families thrive, while going through treatment or facing a terminal illness. Without their support and resources, I honestly don’t know if Evan would have done as well as he did for such a long period of time. I am also currently participating in a grief support group through MaxLove.
How has finding Rett’s Roost been helpful to you?
We were connected with Rett’s Roost very shortly after Evan was diagnosed. Deana has personally been a great support to us. During the pandemic, we were also given a family grant which helped us take an RV trip of a lifetime out west. I have participated in several mom’s outings and in July 2022 we attended a bereavement retreat. Connecting with other families has been so incredibly powerful. Rett’s Roost provides a space for bereaved families to authentically connect with each other and openly grieve.